Conditions Uterine polyps
ICD codes: N84 What are ICD codes?
Growths in the endometrium (uterine lining) often cause spotting or bleeding between menstrual periods (breakthrough bleeding) or after menopause. Uterine polyps are usually harmless. They only have to be removed if they cause discomfort or affect fertility.
At a glance
- Uterine polyps are (mainly benign) growths in the endometrium.
- The most common symptom is bleeding between menstrual periods or after menopause.
- Uterine polyps can go unnoticed.
- The polyps can make it more difficult to get pregnant.
- Uterine polyps are more common with age.
- To obtain a reliable diagnosis and rule out the potential of a malignant condition, the doctor takes a tissue sample for examination.
- Surgery is not always necessary.
Note: The information in this article cannot and should not replace a medical consultation and must not be used for self-diagnosis or treatment.

What are uterine polyps?
Uterine polyps are growths in the endometrium (uterine lining) that are mainly benign. They can be between a few millimeters and a few centimeters in size.
Uterine polyps are more prevalent among postmenopausal women. Their cause is unknown.
Spotting and bleeding between menstrual periods (breakthrough bleeding) or after menopause can be a sign of growths in the endometrium (uterine lining). Polyps sometimes go completely unnoticed though.
Uterine polyps can make it more difficult to get pregnant. In some circumstances, they have to be surgically removed.
What are the symptoms of uterine polyps?
The main symptoms of uterine polyps include spotting and bleeding between menstrual periods, postmenopausal bleeding or bleeding after sexual intercourse. About three-quarters of women with uterine polyps experience some such bleeding. In most cases, only small amounts of blood appear although some women experience a heavier discharge that can be mucous-like or purulent.
Uterine polyps are sometimes asymptomatic and only discovered by chance, for example if a woman seeks medical advice because she is struggling to get pregnant.
What factors increase the risk of uterine polyps?
Uterine polyps are very rare among young women. They become more prevalent with age, especially after menopause. Hormonal changes play a role in this.
Uterine polyps are more common in certain groups than in others, for example women who are obese (severely overweight) or have high blood pressure. Treatment with the drug tamoxifen, which can be used to treat breast cancer, can also increase the risk of uterine polyps.
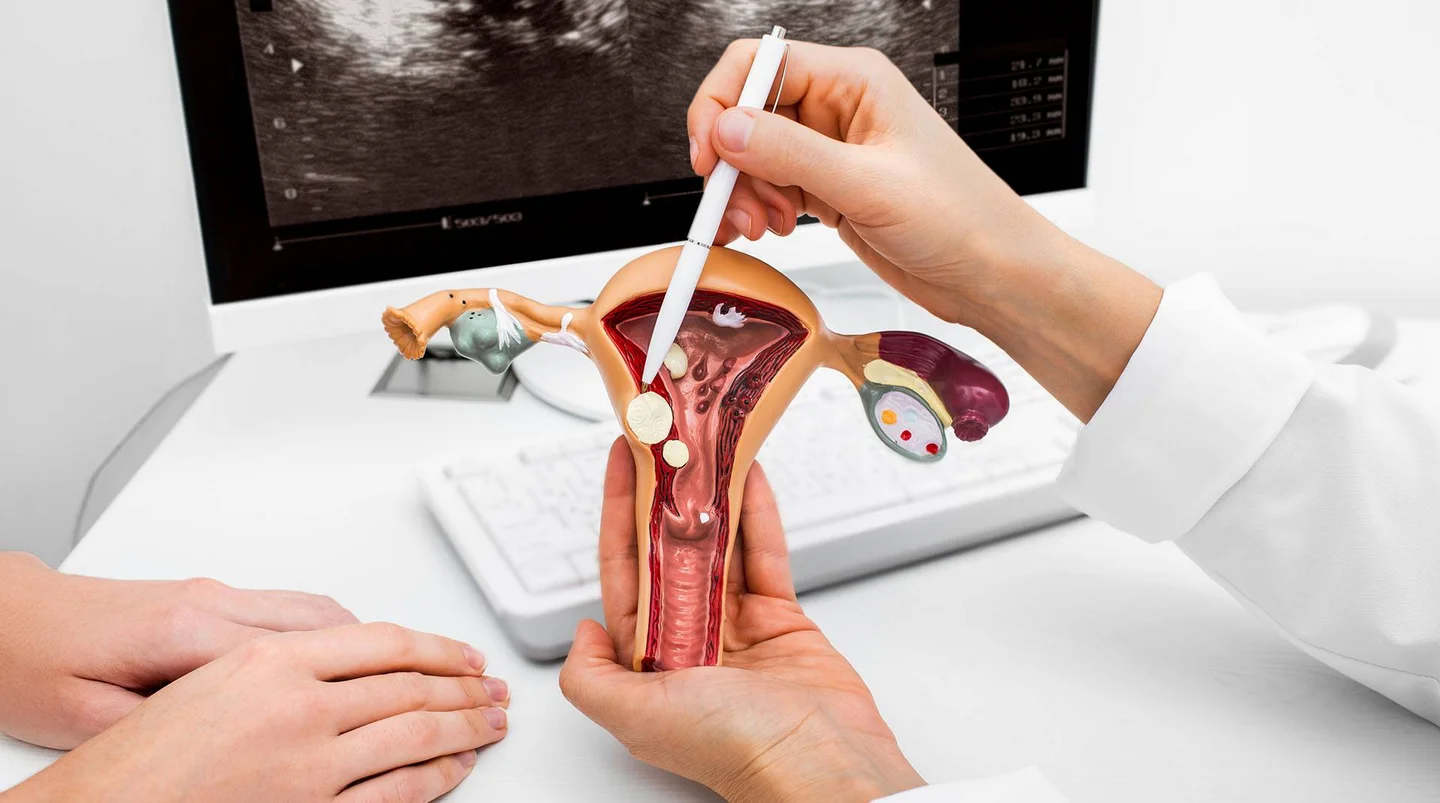
How are uterine polyps diagnosed?
A detailed medical consultation can provide initial indications. The doctor will ask things like whether the patient
- has irregular bleeding
- has previously been or is currently being treated with the breast cancer drug tamoxifen
- takes hormones within the scope of hormone replacement therapy
- is having problems getting pregnant
Polyps in the area of the cervix can sometimes be felt during a gynecological examination. In the case of polyps in the uterus, imaging procedures, such as a vaginal ultrasound or a hysteroscopy (uterine endoscopy), are required. The ultrasound is performed by inserting a rod-shaped probe into the vagina. With a hysteroscopy, the doctor examines the inside of the uterus with an endoscope – a flexible hose or thin metal tube with a camera. Polyps can be removed directly during a hysteroscopy.
For a definitive diagnosis and to rule out the existence of malignant conditions, the removed tissue is examined under a microscope.
How are uterine polyps treated?
Uterine polyps can only be removed surgically. If uterine polyps are asymptomatic and only discovered by chance, surgery is not usually required prior to menopause. However, monitoring is advisable so as to detect any malignant changes at an early stage.
In some cases, it makes sense to remove asymptomatic polyps, for example if:
- there is an increased risk of the polyp becoming cancerous
- the polyp is very large
- the patient has several polyps at the same time
- the polyp protrudes into the cervix
- the patient wants to get pregnant but is struggling to do so
Uterine polyps that cause problems should always be removed.
Uterine polyps are usually removed during a hysteroscopy: The doctor removes the polyps with an endoscope, which is introduced into the uterus through the vagina. The endoscope has a light and a camera. Surgical instruments can be inserted via a small channel in the endoscope. The camera can be used to externally control the intervention. The polyp removal procedure (polypectomy) is usually straightforward.
- DynaMed (Internet), Ipswich (MA). Endometrial Polyp. EBSCO Information Services. Record No. T113946. 2018 (1995). Aufgerufen am 21.02.2022.
- Norwegian Society of Obstetrics and Gynecology. Endometrial polyps. 2015.
- UpToDate (Internet). Approach to abnormal uterine bleeding in nonpregnant reproductive-age patients. Wolters Kluwer 2021. Aufgerufen am 21.02.2022.
- UpToDate (Internet). Endometrial Polyps. Wolters Kluwer 2021. Aufgerufen am 21.02.2022.
In cooperation with the Institute for Quality and Efficiency in Health Care (Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen – IQWiG).
As at:


