Conditions Pleural effusion
ICD codes: J90 J91 What are ICD codes?
Symptoms of pleural effusion include shortness of breath, coughing and chest pain. Pleural effusion is caused by certain conditions that lead to an increased build-up of fluid in the pleural space – the narrow space between the lungs and the chest wall. The fluid can be drained if necessary.
At a glance
- Pleural effusion is a build-up of fluid between the pleura – these are the thin membranes lining the outside of the lungs and the inside of the chest cavity.
- The two membranes are called the “visceral pleura”, which lines the outside of the lungs, and the “costal pleura”, which lines the inside of the chest cavity.
- The space between these two membranes is known as the pleural space and, if fluid collects here, it causes chest pain and shortness of breath that can reach the point of respiratory distress (dyspnea).
- Pleural effusion is caused by other conditions such as heart failure or a lung infection/pneumonia.
- Mild pleural effusion often clears up on its own.
- If the symptoms are acute, doctors can drain fluid from the pleural space.
Note: The information in this article cannot and should not replace a medical consultation and must not be used for self-diagnosis or treatment.

What is pleural effusion?
Pleural effusion is the build-up of fluid, pus or blood in the pleural space. Pleural effusion is sometimes also called “water on the lungs”, although this name is also given to a different condition, i.e. pulmonary edema. The pleural space is a narrow, fluid-filled area between the two membranes that cover the outside of the lungs (the visceral membrane) and the inner wall of the chest (the costal membrane).
In pleural effusion, there is an excessive build-up of fluid in the pleural space – the area between the pleura. These two membranes are called the “visceral pleura”, which lines the outside of the lungs, and the “costal pleura”, which lines the inside of the chest cavity.
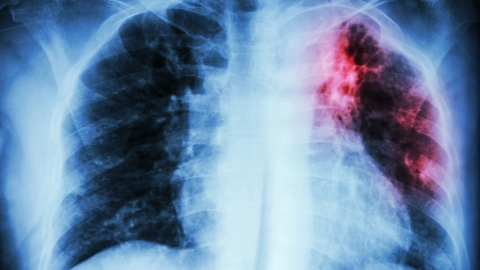
Shortness of breath, coughing and chest pain may all be symptoms of pleural effusion. However, some people with pleural effusion experience no symptoms at all. Doctors can identify a build-up of fluid on a chest X-ray.
Pleural effusion is very common and always occurs in connection with another condition, such as:
- heart failure (cardiac insufficiency)
- lung infection (pneumonia)
- pulmonary embolism
- malignant tumors, e.g. lung or breast cancer
- broken ribs
The underlying condition is treated as a priority, where possible. Mild pleural effusion often clears up on its own. With severe pleural effusion, doctors can drain the excess fluid from the pleural space.
What are the symptoms of pleural effusion?
People may experience the following symptoms of pleural effusion, depending on how much fluid has collected in the pleural space:
- shortness of breath that can reach the point of respiratory distress (difficulty breathing)
- coughing
- chest pain
They may also have a high temperature, cough up bloody sputum (mucus) and lose weight.
Additional symptoms may also occur, depending on what exactly is causing the excess fluid to collect in the pleural space:
- shortage of oxygen or water retention (e.g. in the legs) due to heart failure
- high temperature, chills and coughing due to a lung infection (pneumonia)
- respiratory distress and chest pain due to a pulmonary embolism
In some cases, pleural effusion only causes mild symptoms or produces no symptoms at all.
What causes pleural effusion?
In a healthy individual, the volume of fluid absorbed into the pleural space is the same as the volume of fluid that is produced – in other words, there is a fluid balance. With pleural effusion, this balance is disturbed and more fluid is produced than can be absorbed. This results in an excessive build-up of fluid.
Pleural effusion is often caused by underlying conditions such as heart failure or pulmonary embolism. However, it can also occur as a result of broken ribs or following a surgical procedure.
In addition, bacterial and (more rarely) viral infections of the lungs can also lead to pleural effusion. These include:
- lung infection (pneumonia)
- tuberculosis (TB)
- infection with HIV
- infection with the SARS-CoV-2 coronavirus
Pleural effusion can also develop in connection with various types of cancer, such as:
- lung cancer
- breast cancer
- stomach and bowel cancer
- ovarian cancer
Other possible but rare causes are:
- cirrhosis of the liver
- diseases of the kidneys
- acute or chronic inflammation of the pancreas (pancreatitis)
- chronic inflammatory rheumatoid arthritis
- various types of medication
- inhaling asbestos and other substances that are damaging to the lungs
How common is pleural effusion?
Pleural effusion is relatively common because it can occur as an accompanying symptom of various other conditions. Between 1 and 5 out of 1,000 people are estimated to develop pleural effusion in Germany every year.
How is pleural effusion diagnosed?
If the symptoms a patient is experiencing are suggestive of pleural effusion, the doctor will begin by taking a detailed medical history to pinpoint symptoms, underlying conditions, any medication the patient is taking and any recent surgical procedures.
Various tests will then be conducted, based on the underlying condition in each case, as well as on the type and severity of the symptoms:
- listening to the lungs
- taking a chest X-ray
- listening to the heart or performing an ultrasound scan of the heart
Some of the accumulated fluid from the pleural space is removed using a fine needle (this procedure is known as aspiration or diagnostic thoracentesis).
It is rarer for computed tomography (CT) to be used but this may be done in the case of unclear results or severe infections. If the cause of the pleural effusion is an infection, the fluid collected is analyzed in the lab to identify the potential pathogens (disease-causing organisms) involved.
How is pleural effusion treated?
If pleural effusion causes acute respiratory distress or acute heart problems, this must be treated as an emergency. In this situation, it is imperative to dial 112 to alert emergency services. Doctors then use a tube to drain the excessive fluid and reduce pressure in the chest cavity. This procedure is known as pleural fluid draining (or as aspiration, therapeutic thoracentesis or pleural tapping).
If the cause is a bacterial lung infection, this can be treated with antibiotics. If the cause is heart failure, diuretic medication (diuretics) can provide relief. In many cases, the symptoms then subside.
Cancer may cause recurring pleural effusion. In this case, the patient will need to have pleural fluid draining performed on a regular basis. Alternatively, the doctor can insert a pleural catheter into the pleural space to drain excessive fluid. The visceral membrane on the outside of the lungs can then be surgically connected to the costal membrane on the inside of the chest wall. The medical term for this procedure is pleurodesis. It prevents fluid from collecting in the area again – or at least reduces the risk of this happening.
- DynaMed [Internet], Ipswich (MA). Pleural Effusion. EBSCO Information Services. Record No. T474331. 2018 (1995). Aufgerufen am 11.03.2021.
- Jany B, Welte T. Pleural Effusion in Adults – Etiology, Diagnosis, and Treatment. Dtsch Arztebl Int 2019. Aufgerufen am 11.03.2021.
- UpToDate (Internet). Diagnostic evaluation of a pleural effusion in adults: Initial testing. Wolters Kluwer 2020. Aufgerufen am 11.03.2021.
- UpToDate (Internet). Management of nonmalignant pleural effusions in adults. Wolters Kluwer 2020. Aufgerufen am 11.03.2021.
- UpToDate (Internet). Management and prognosis of parapneumonic pleural effusion and empyema in adults. Wolters Kluwer 2020. Aufgerufen am 11.03.2021.
In cooperation with the Institute for Quality and Efficiency in Health Care (Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen – IQWiG).
As at: