Conditions Heart palpitations (due to paroxysmal atrial tachycardia)
ICD codes: I47.1 What are ICD codes?
Paroxysmal atrial tachycardia is when a person's heart suddenly beats very fast. It lasts for a few minutes and stops again just as quickly. There are simple things people can do to end an episode themselves.
At a glance
- Paroxysmal atrial tachycardia is when a person's heart suddenly beats very fast.
- It lasts for a few minutes and disappears again just as quickly.
- This arrhythmia doesn’t usually have any serious complications.
- There are simple things people can do to end an episode themselves.
Note: The information in this article cannot and should not replace a medical consultation and must not be used for self-diagnosis or treatment.

What are heart palpitations (tachycardia)?
Even healthy people’s hearts sometimes beat very fast when they are exercising or under stress – this is perfectly normal. However, when “heart palpitations” or a “rapid heartbeat” (tachycardia) are experienced, the heart beats very quickly due to illness.
This article discusses heart palpitations due to paroxysmal atrial tachycardia (paroxysmal supraventricular tachycardia). With this condition, the heart suddenly beats very fast. The heartbeat is too fast, but it remains regular. The heart palpitations usually settle on their own after a while. This form of arrhythmia does not usually have any serious complications.
However, there are other, more serious conditions that can cause heart palpitations, including atrial fibrillation. In such cases, the heartbeat is also irregular.
What are the symptoms of heart palpitations caused by paroxysmal atrial tachycardia?
If the heart suddenly beats very fast, it can often be felt as a racing heart (tachycardia) or palpitations. The heart rate is usually between 180 and 200 beats per minute. But it can also be slightly below or above that. This can be alarming and uncomfortable. Possible symptoms are dizziness, nausea, chest pain, and shortness of breath. More rarely, people may faint (syncope) and fall as a result. Some people have to pass a lot of urine after an episode.
Important: Life-threatening complications are very rare with paroxysmal atrial tachycardia.
What are the causes of heart palpitations?
For a healthy person, how often the heart beats depends on their physical and psychological stress levels. For example, exercise, stress or feeling nervous make the heart beat faster. The sinus mode in the right atrium controls how the heart rate adapts to the additional strain.
With paroxysmal atrial tachycardia, the cause of rapid heart is usually a disruption of the AV node. This is located between the atria and ventricles. If the AV node is working normally, it conducts impulses from the atria to the ventricles.
In people with atrial tachycardia, this conduction may be disrupted. If this happens, impulses become “trapped” in the AV node, where they continue to move in a circular pathway. The AV node then transmits too many impulses to the ventricles. This means that the heart beats very fast.
The condition may also occur if a person is born with additional conduction pathways between the atria and ventricles. These form a short circuit, so that an impulse is conducted into the ventricles but is also conducted back in the direction of the atria and may then move in a loop between the ventricles and atria.
Fast defective impulses can also cause this. They develop in the atria and trigger a heartbeat that is too rapid.
Another possible trigger is a heartbeat that occurs outside of the heart’s normal rhythm (this is known as an extrasystole). Extrasystoles also occur in healthy people every now and then spontaneously and do not cause any symptoms.
Heart palpitations can also be caused by changes in a person’s salt intake or consumption of alcohol or drugs.
How common are heart palpitations due to paroxysmal atrial tachycardia?
Approximately 2 to 3 people in every 1,000 have heart palpitations originating in the atrium or at the junction of the atrium and ventricle. Atrial tachycardia is more common in women than men. The risk increases with age.
However, the condition occurs more often in men and younger people when it is due to additional conduction pathways between the atria and ventricles present at birth.
Usually an episode comes on suddenly, lasts for a few minutes and disappears just as suddenly as it came. For some people, however, the heart palpitations may last for more than an hour.
The time between episodes can vary – some people have several episodes a day, while others have episodes days, weeks or months apart.
How are heart palpitations diagnosed?
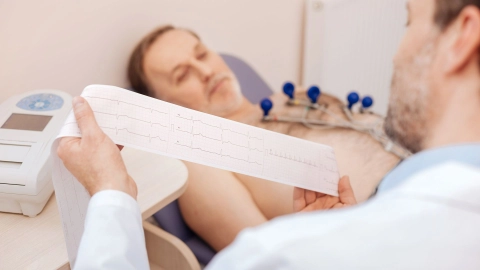
The typical symptoms and how they develop usually already indicate paroxysmal atrial tachycardia. But an electrocardiogram (ECG) is needed to make a clear diagnosis, as with all arrhythmias. However, as an episode will not always occur when the person is connected to an ECG device, 24-hour ECG monitoring is often used.
Other tests can be conducted to determine the exact causes and rule out more serious arrhythmias – for instance, a heart ultrasound (echocardiography) or a thyroid test. A special heart catheterization can be used to examine whether there are innate additional conduction pathways between the atria and the ventricles.
How are heart palpitations due to paroxysmal atrial tachycardia treated?
To treat heart palpitations due to paroxysmal atrial tachycardia, doctors first need to rule out serious arrhythmias that require different treatments.
People who are otherwise healthy and for whom an occasional rapid heartbeat is not a problem do not usually need any treatment.
There are also simple things people can do to end an episode themselves. For example, it may help to quickly drink a cold glass of water. A special breathing technique known as the Valsalva maneuver has proven to be particularly effective. It involves increasing pressure in the abdomen by breathing in and pressing on the stomach, −as though trying to suppress a hiccup. It is often combined with certain postures, such as holding the legs in a raised position. The maneuver stimulates the vagus nerve – a nerve that sends signals to the heart and can slow the heart rate.
These measures are also the first to be used in medical practices or hospitals. Medication is only injected when they do not work. It’s rare for an episode to have to be ended by an electric shock (cardioversion).
If the episodes are very stressful for those affected, there is the option of permanently suppressing them. Medication or cardiac catheterization will be considered.
For more detailed information, e.g. about home remedies for heart palpitations, see gesundheitsinformation.de.
- Brandes R, Lang F, Schmidt R. Physiologie des Menschen: mit Pathophysiologie. Berlin: Springer; 2019.
- Brugada J, Katritsis DG, Arbelo E et al. 2019 ESC Guidelines for the management of patients with supraventricular tachycardia. The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J 2020; 41(5): 655-720. Aufgerufen am 13.06.2023.
- Hindricks G, Hoffmann E, Kuck KH et al. Kommentar zu den Leitlinien (2019) der ESC zur Behandlung supraventrikulärer Tachykardien. Kardiologe 2021; 15: 194-200. Aufgerufen am 13.06.2023.
- Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J. Harrison's Principles of Internal Medicine. McGraw-Hill: New York 2015. Aufgerufen am 13.06.2023.
- Lan Q, Han B, Wu F et al. Modified Valsalva maneuver for treatment of supraventricular tachycardias: A Meta-analysis. Am J Emerg Med 2021; 50: 507-512. Aufgerufen am 13.06.2023.
- Page RL, Joglar JA, Caldwell MA, Calkins H, Conti JB, Deal BJ et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2016. 67(13): 1575-1623. Aufgerufen am 13.06.2023.
- Siegenthaler W, Blum HE (Ed). Klinische Pathophysiologie. Thieme: Stuttgart 2006.
- Smith GD, Fry MM, Taylor D, Morgans A, Cantwell K. Effectiveness of the Valsalva Manoeuvre for Reversion of Supraventricular Tachycardia. Cochrane Database Syst Rev 2015; (2): CD009502. Aufgerufen am 13.06.2023.
- Wood KA, Wiener CL, Kayser-Jones J. Supraventricular tachycardia and the struggle to be believed. Eur J Cardiovasc Nurs 2007. 6(4): 293-302. Aufgerufen am 13.06.2023.
In cooperation with the Institute for Quality and Efficiency in Health Care (Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen) (IQWiG).
As at: