Conditions Measles
ICD codes: B05 What are ICD codes?
Measles is a very contagious viral infection that causes fever and a distinctive skin rash. Serious complications such as encephalitis can occur, particularly in infants and older people. Vaccination protects against a severe infection.
At a glance
- Measles is a viral infection accompanied by a fever.
- A distinctive skin rash indicates measles.
- Serious complications can arise. These include, in particular, encephalitis (inflammation of the brain), which can cause permanent damage or death.
- Vaccination provides effective protection.
- As of March 2020, proof of sufficient protection against measles is mandatory. This applies, for example, to people born after 1970 who are working in healthcare or community facilities or who are being cared for in a community facility.
Note: The information in this article cannot and should not replace a medical consultation and must not be used for self-diagnosis or treatment.


What is measles?
Measles is a highly contagious viral infection that affects both children and adults. Measles causes a skin rash that starts on the face and spreads over the entire body.
Measles can cause serious complications. For example, it can lead to inflammation of the brain (encephalitis) which is fatal in 10 to 20 percent of cases.
Vaccination generally prevents measles. For people born after 1970 who are working in healthcare or community facilities, such as kindergartens or hospitals, proof of sufficient protection against measles has been mandatory since March 2020. This also applies to children and adolescents attending community facilities. A person is protected against measles if they have been vaccinated or have recovered from a prior infection.
What are the symptoms of measles?
A measles infection progresses in two phases. The distinctive skin rash appears in the second phase of the illness.
Phase 1
Initial symptoms appear approx. 10 days after contracting the virus. The infection starts with a fever, inflammation of the eyes (conjunctivitis), sneezing, an itchy and blocked or runny nose, and coughing. White patches (Koplik spots) form on the lining of the mouth inside the cheeks. These look like tiny grains of chalk and are a disease-specific sign of measles.
Phase 2
Approximately 2 to 4 days after the onset of the first symptoms, a distinctive skin rash appears, with brown-red spots that come together to form one mass. The rash starts on the face and behind the ears and spreads over the entire body. It lasts for about 4 to 7 days. It often leaves behind small patches of skin that peel off in scales. The fever lasts for approximately one week.
Important: Infected individuals are contagious as early as 4 days before the skin rash appears. This contagious period lasts for 4 more days. The risk of infecting others is greatest shortly before the skin rash appears.
How do people become infected with measles?
The pathogen responsible for causing measles is the measles virus (morbilli virus). This type of virus is found only in humans. Therefore, measles can only be passed from human to human.
Measles are highly contagious – almost anyone who comes in contact with a person with measles becomes infected. And almost anyone who becomes infected will fall ill. Anyone who has had the infection acquires lifelong immunity. This means that people cannot contract measles twice. Anyone who has been vaccinated against measles is general also immune. In a very small number of cases, people who have received a vaccine can contract a mild measles infection without serious complications.
Droplet infection
One way in which measles is spread is via droplet infection. This happens when someone talks, sneezes, or coughs. If the droplets released are inhaled by a healthy individual and reach the mucous membranes of their airways, that person becomes infected.
Aerosol infection
Microscopic droplets (aerosols) that circulate in the air can also cause infection within enclosed spaces. This can even occur hours after the infected individual has left the room.
Smear infection
The infection can also be contracted by touching hands, objects or surfaces that have been contaminated by infectious secretions from the nose and throat of an infected individual.
How common is measles?
Measles cases can be found throughout the world, especially in countries where few people are vaccinated against the virus. There, almost every person will contract the virus infection at some stage of their life. Therefore, measles is a frequent cause of death in children globally, in particular in countries where vaccination rates are low and people don’t receive adequate nutrition.
Every year in Germany, between 3 and 7 people die of measles or its complications. Here, the prevalence of the measles infection has sharply declined because most children are vaccinated. Nevertheless, there are occasionally regional outbreaks, primarily among insufficiently vaccinated groups.
Measles is considered a childhood disease. However, it has been observed over recent years that more than half of those infected are aged 15 or older. This is due to inadequate immunity among this age group. In addition, children younger than one year old can also contract the virus before they have received a vaccination.
The goal is to eradicate measles completely through consistent vaccination. This has already been achieved in some countries with high vaccination rates.
What complications are associated with measles?
A measles infection is often followed by bacterial infections. Life-threatening complications may also arise if the brain becomes inflamed (encephalitis).
Subsequent bacterial infections
The measles virus triggers an immune deficiency that lasts several months. The immune system may also be weakened for a number of years following a measles infection. Therefore, patients can also become infected by bacteria during this time.
Typical secondary disorders that can result after a measles infection are:
Measles encephalitis
Acute encephalitis (measles encephalitis) occurs in one out of 1,000 measles cases. 10 to 20 percent of those affected will die as a result. In 20 to 30 percent of people, the encephalitis results in permanent damage, such as cognitive impairment or paralysis.
Rare late complications
In rare cases, slowly progressive encephalitis (subacute sclerosing panencephalitis – SSPE) occurs 6 to 8 years after a measles infection. It is generally fatal. SSPE starts with psychological and intellectual changes and ends with a loss of all brain functions. The risk of developing SSPE is particularly high among children.
Video Are childhood diseases dangerous?
The video below outlines the most common childhood diseases and the symptoms they present.
This and other videos can also be found on YouTube
Watch nowThe privacy policy indicated there applies.
How can measles be prevented?
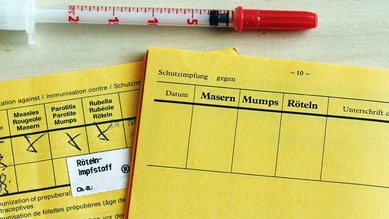
Vaccination offers protection against measles. Typically, the vaccination is administered as part of a combined live virus vaccine (MMR) that also protects the person from mumps and rubella. There is also a vaccine (MMRV) that offers additional protection against chickenpox (varicella).
The German Standing Committee on Vaccination (STIKO) of the Robert Koch Institute recommends the following vaccination schedules:
Vaccination for children
Children should normally receive their first measles vaccination at the age of 11 months. A second vaccination is required at 15 months. The minimum amount of time between the first and second vaccination is 4 weeks. The second dose provides lifelong protection without the need for a booster.
Vaccination at 9 months is possible if the child is attending a community facility. In this case, it is recommended that the second dose of MMR vaccine is given shortly after the child turns 1.
Important: According to the Measles Protection Act (“Masernschutzgesetz”) children from the age of 1 must have received at least one vaccine dose if they are attending a community facility. Proof of having received two vaccine doses is then required once the child turns 2. Alternatively, proof that the child has previously had a measles infection or documentation that they cannot be vaccinated against measles for medical reasons will suffice.
Vaccination for adults
A single vaccine against measles is recommended for adults born after 1970 if the following criteria apply:
- they were never vaccinated against measles
- they only received one vaccine dose against measles during childhood
- their vaccination status is unclear
Two vaccines against measles are recommended for people born after 1970 who work in certain sectors. This applies to people employed in:
- healthcare, community or care facilities
- technical and vocational colleges and institutions of higher education
- community accommodation for refugees and asylum seekers
Video How do vaccinations work?
The video below explains how a vaccination works.
This and other videos can also be found on YouTube
Watch nowThe privacy policy indicated there applies.
Reactions to the vaccination
Following vaccination, people may sometimes have a reaction and experience redness, swelling, and pain around the site of the injection. General symptoms, such as fever, headaches, and aching limbs can occur, but subside after a few days. A rash similar to the rash that occurs with a measles infection occurs in around 5 percent of those who receive the vaccine. This vaccination rash is mild, clears up after a few days, and is not contagious.
To find out whether vaccination against measles is recommended for you or your child, consult the Impfcheck vaccination checker tool from the Federal Center for Health Education (Bundeszentrale für gesundheitliche Aufklärung, BZgA).
The website of the Robert Koch Institute provides answers to frequently asked questions about the measles vaccination.
What does the Measles Protection Act (“Masernschutzgesetz”) have to say?
The Measles Protection Act seeks to improve protection against measles in community facilities and in medical facilities. Community facilities include, for example, kindergartens and schools. The premises of daycare providers are also included in this category under infection legislation.
The Measles Protection Act stipulates that certain groups of people must provide proof of sufficient protection against measles. They must have documentation of having received two measles vaccines or having recovered from a measles infection in the past. In certain cases, people are permitted to go without an MMR vaccination for medical reasons. However, documentation must be provided.
According to the Measles Protection Act, people are required to provide proof of sufficient protection against measles if they were born after 1970 and work in certain sectors. This applies to people employed in:
- healthcare, community or care facilities
- technical and vocational colleges and institutions of higher education
- community accommodation for refugees and asylum seekers
The obligation to provide proof also applies to apprentices, trainees, students on placement and volunteers working in these areas.
In addition, asylum seekers and refugees are required to provide proof of adequate protection against measles within 4 weeks of being accepted into community accommodation.
The following rules apply to children under the Measles Protection Act:
- Children from the age of 1 must have proof of vaccination against measles in order to attend a community facility.
- Proof of two measles vaccines is required as of the age of 2.
Further information about the Measles Protection Act is available on the information pages of the Federal Center for Health Education (Bundeszentrale für gesundheitliche Aufklärung – BZgA).
How is measles diagnosed?
The symptoms of measles are not always disease-specific. They are very similar to those of other viral illnesses with a skin rash, such as rubella or scarlet fever. For a reliable diagnosis, doctors take a throat swab or urine sample for laboratory analysis. It is also possible to detect the measles virus indirectly via antibodies in the blood. For this purpose, doctors take a blood sample and send it to a lab for analysis.
How is measles treated?
Once a measles infection is detected, its treatment depends on the patient.
Treating the acutely ill
There is no specific treatment for the measles virus. For people with measles in its acute stage, bed rest is needed. Pain medication that lowers fever and has an anti-inflammatory effect can be taken to treat fever and cold-like symptoms. If other bacterial infections occur, doctors will prescribe antibiotics.
Important: Those with acute cases of measles may not attend or work at a community facility within the first 5 days of the onset of a skin rash. The precise period is defined by the doctor who is treating the patient.
Treatment of contacts
All contacts from the age of 9 months with no vaccination protection or with unknown immunity should be vaccinated once against measles within 3 days of contact with an infected person. This helps to prevent an outbreak of the illness or at least a severe case. It is also possible for infants aged 6 of 8 months to receive a vaccination following contact with an infected person, subject to consideration of the individual circumstances.
No special measures apply to fully vaccinated contacts. The same applies to people who have recovered from a prior infection with measles.
Attending or working at a community facility
Contacts may enter a community facility, such as a childcare facility or school, only if they have been sufficiently vaccinated prior to a possible infection. Alternatively, they can be vaccinated within 3 days of contact. Otherwise, they must not enter the community facility for 3 weeks.
Passive immunization of high-risk patients
Patients with a weakened immune system, pregnant women, and infants under the age of 6 months are at an increased risk of developing measles with complications and are unable to receive a vaccination. They may be given antibodies against the virus within 6 days of contact to protect them from the infection. The sooner that the antibodies can be administered after contact, the more effective the protection they offer against the disease.
Where can more information about measles be found?
Detailed information about measles and the Measles Protection Act can be found at masernschutz.de, a service provided by the Federal Center for Health Education (Bundeszentrale für gesundheitliche Aufklärung – BZgA).
Further information about the measles vaccines that are recommended for children, adolescents, and adults is available from the website of the Federal Center for Health Education (Bundeszentrale für gesundheitliche Aufklärung, BZgA) at impfen-info.de.
- Bundeszentrale für gesundheitliche Aufklärung (BZgA). Erregersteckbrief: Masern. infektionsschutz.de. Aufgerufen am 15.01.2025.
- Bundeszentrale für gesundheitliche Aufklärung (BZgA). Rechtliche Aspekte. masernschutz.de. Aufgerufen am 15.01.2025.
- UpToDate (Internet). Measles: Clinical manifestations, diagnosis, treatment, and prevention. Wolters Kluwer 2024. Aufgerufen am 15.01.2025.
- Robert Koch-Institut (RKI). RKI-Ratgeber: Masern. Aufgerufen am 15.01.2025.
- Weltgesundheitsorganisation (WHO). Eliminierung von Masern und Röteln und Prävention der kongenitalen Rötelninfektion Strategie der Europäischen Region der WHO 2005–2010. 2005.
Reviewed by the German Society for Pediatric Infectiology (Deutsche Gesellschaft für Pädiatrische Infektiologie e.V.).
As at: