Conditions Mumps
ICD codes: B26 What are ICD codes?
Mumps is a contagious viral infection typically characterized by a high temperature and painful swelling of the parotid glands. Complications such as inflammation of the meninges or testicles are possible, especially in adolescents and adults. Vaccination protects against the disease.
At a glance
- Mumps is a viral infection accompanied by fever.
- The condition is typically characterized by painful swelling of the parotid glands.
- Mumps is usually contracted by “droplet infection”, especially when speaking, sneezing or coughing.
- Mumps can be associated with complications such as inflammation of the mammary glands, the testicles and the meninges (brain membranes).
- The typical age of infection has changed to teens and young adults.
- Vaccination protects against the disease.
Note: The information in this article cannot and should not replace a medical consultation and must not be used for self-diagnosis or treatment.

What is mumps?
Mumps is a contagious viral infection that affects not only children, but also adults. Typical symptoms are painful, swollen parotid glands between the masticatory muscle and the ear. In particular, teens and adults can be affected by complications such as testicular inflammation or meningitis and deafness.
Important: In Germany, the prevalence of this infection has sharply declined since the nationwide vaccination of children against mumps. However, the typical age of infection has changed to adolescence and young adulthood.
What are the symptoms of mumps?
Initial symptoms can include a headache, aching limbs, a high temperature and a loss of appetite. Painful swelling of the parotid glands is typical for the condition. As these are located in front of the ears, the cheeks can appear swollen. The parotid glands can be swollen on one or both sides. In some cases, the salivary glands on the lower jaw and under the tongue are also affected.
Some people with mumps can have no symptoms or symptoms that are similar to those of a common cold. This is especially true in the case of infants.
Which pathogens cause mumps?
Mumps is caused by the mumps virus and is found globally. The virus occurs only in humans, therefore mumps is always transmitted only from human to human.
How do people become infected with mumps?
The mumps virus is spread via “respiratory droplets”. Tiny droplets from the nose and mouth contain the virus and are distributed in the air. This happens when someone talks, sneezes, or coughs. Other people become infected with the virus through the air or direct contact with saliva. Transmission through objects that have the virus on their surface is rather rare.
Who can contract mumps?
Anyone who has not obtained sufficient immunity through vaccination or a previous infection can contract mumps.
Important: On rare occasions, even people who have been fully vaccinated with two vaccine doses can sometimes contract mumps. In such cases though, the illness tends to be milder than in those who have not been vaccinated.
How common is mumps?
Mumps is found throughout the world. In Germany, the prevalence of the mumps infection has sharply declined because most children are vaccinated. However, outbreaks do still occasionally occur. In recent years, an average of 500 mumps infections per year have been reported in Germany. The typical age of infection has changed from 5 to 9 years to adolescence and young adulthood.
How does mumps progress?
Initial symptoms appear between approx. 2 to 3 weeks after infection with the virus. The swelling of the parotid glands lasts for around 3 to 8 days.
Patients are contagious as early as 7 before to 9 days after the swollen parotid glands appear. Even infected persons without symptoms can transmit the virus.
What complications can occur with mumps?
The older the patient, the more often complications appear.
Effects on the central nervous system
The illness can be accompanied by symptoms affecting the central nervous system (CNS). These usually occur several days after the parotid glands swell but can also occur prior to this or be the only symptom of the illness.
These include:
- encephalitis (less than 1 percent) with paralysis; can be fatal in rare cases
- meningitis (up to 10 percent) with severe headaches, stiff neck and vomiting, however without permanent injury
- temporary loss of hearing of high tones (approx. 4 percent)
- permanent deafness in one ear (1 in 20,000 people with mumps)
Testicular inflammation
Testicular inflammation in one or both testicles can appear approx. 4 to 8 days after the swollen parotid glands and lasts one to two weeks. The fever spikes again and the testicles become swollen and painful. Approximately 15 to 30 percent of infected male teens and adults are affected. In rare cases, testicular inflammation can lead to infertility.
Inflammation of the breasts and ovaries
Up to 30 percent of infected women experience an infection of the mammary glands, and up to 5 percent experience an infection of the ovaries. Contrary to previous assumptions, mumps in pregnant women does not increase the child’s risk of birth defects.
Further possible complications
Further possible complications related to mumps include:
- pancreatitis
- inflammation of the kidneys
- arthritis
- anemia
- myocardial inflammation
Are childhood diseases dangerous?
The video below outlines the most common childhood diseases and the symptoms they present.
This and other videos can also be found on YouTube
Watch nowThe privacy policy indicated there applies.
How can mumps be prevented?
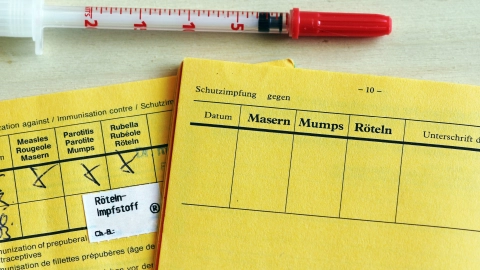
A vaccination can provide protection from mumps. The German Standing Committee on Vaccination (STIKO) of the Robert Koch Institute recommends the following procedure:
Vaccination for children
Children should receive their first mumps vaccination between the ages of 11 to 14 months. A second vaccination is required between the age of 15 and 23 months. The minimum amount of time between the first and second vaccination is 4 weeks. Missed vaccinations should be administered by the age of 18. The second dose provides lifelong protection without the need for a booster.
Vaccination for adults
Adults born after 1970 who work in certain professions should also receive two doses of the mumps vaccine. This includes personnel in medical and care facilities, community facilities and communal accommodation facilities, for example for refugees, as well as staff in technical and vocational colleges and higher education institutes.
Typically, vaccination occurs in the form of a combined live virus vaccine (MMR) that also provides protection against measles and rubella. Doctors can also administer a vaccine (MMRV) that offers additional immunity against chickenpox (varicella).
The website of the Robert Koch Institute provides answers to frequently asked questions about the mumps vaccination.
Video How do vaccinations work?
The video below explains how a vaccination works.
This and other videos can also be found on YouTube
Watch nowThe privacy policy indicated there applies.
What should you do if you come into contact with someone who has mumps?
Anyone who has not been vaccinated, who only received one vaccine dose during childhood or whose vaccination status is unclear should receive a single MMR vaccine dose following contact with someone who has mumps. This should occur within 3 days of the contact.
How is mumps diagnosed?
Mumps is often diagnosed by the typical swelling of the parotid glands. If mumps is suspected, the virus should always be confirmed in a laboratory. Doctors can do this through the use of either a throat swab or a urine sample. Furthermore, virus antibodies can be found in a blood sample.
How is mumps treated?
There is no special treatment for the mumps virus. Pain medication that lowers fever and has an anti-inflammatory effect can be taken to treat symptoms such as fever and painful swelling of the parotid glands.
- Bundeszentrale für gesundheitliche Aufklärung. Erregersteckbrief: Mumps. Aufgerufen am 18.11.2024.
- Robert Koch-Institut (RKI). Epidemiologisches Bulletin 25.01.2024. Aufgerufen am 18.11.2024.
- Robert Koch-Institut (RKI). RKI-Ratgeber: Mumps. Aufgerufen am 18.11.2024.
- Robert Koch-Institut (RKI). SurvStat@RKI 2.0. Web-basierte Abfrage der Meldedaten gemäß Infektionsschutzgesetz (IfSG). Aufgerufen am 18.11.2024.
Reviewed by the German Society for Pediatric Infectiology (Deutsche Gesellschaft für Pädiatrische Infektiologie e.V.).
As at: